The Centers for Disease Control and Prevention has recognized that people with HIV are at a greater risk for severe disease and death than those without HIV, when hospitalized with coronavirus disease 2019 (COVID-19).1–3 It is also known that individuals with neurological conditions such as dementia are also at a higher risk for severe outcomes with COVID-19.4 The basis for including neurological comorbidities was a study that used International Classification of Diseases (ICD) revision 10 billing coding.4 Such codes allow a quick understanding of a large volume of data. However, around 40% of people in the USA who have dementia are not coded.5 The people missed are likely to be non-English speaking, have some other barrier to care or have other comorbidities such as HIV, in which individuals have cognitive concerns at a younger age than we would traditionally consider for dementia (about 65 years). Dr Mukerji therefore hypothesized that other forms of cognitive classification, such as cognitive concerns, are a useful means of classifying persons at risk for severe disease in COVID-19, especially among people with HIV. The subsequent study was presented during IDWeek, 19–23 October 2022.6
In this expert interview, Dr Mukerji describes her recent study and its implications for future clinical practice.
Q. What were the aims, design and eligibility criteria of the study that you presented?
The aims were to decide whether individuals with dementia or cognitive concerns were at risk of death from COVID-19, and to determine the effects of dementia and cognitive concerns in a subpopulation with HIV. We verified a set of ICD codes that covered dementia and cognitive impairment in the USA but also used the wider definition of people who had announced to their healthcare provider that they had cognitive concerns. It was a single-site case-control study, though Massachusetts General Hospital is very large and has three tertiary centres. We had electronic records for around 14,000 people with COVID-19. Among this population, we identified a subgroup with HIV and COVID-19 that we matched to a control group on factors including age, race, ethnicity and ZIP code. The timescale was from March 2020 to April 2021.
Q. What were the findings of the study?
ICD billing codes are a quick and easy way to categorize individuals but they carry a risk of misclassification. It can take a long time to review clinical notes and difficulties can be encountered when establishing a standardized work flow. We had previously designed a software tool that could pull together unstructured clinical notes, lab values and medications, to present them in an accessible manner so that neurologists can easily decide whether or not the patient had a cognitive concern. We are hoping to promote this tool in large practices to classify people more precisely than the ICD code. In our small cohort of people with HIV (64 people), we found that cognitive concern is a risk factor for severe COVID-19 outcomes. People with HIV had an increased risk of death from COVID-19 (17.2%) versus people without HIV (6.3%). The Veterans Aging Cohort Study index 2.0 was found to be a good predictor of COVID-19 outcomes in the total cohort of people analysed (527 people). Dementia as an ICD code had a twofold increased risk for mortality from COVID-19. Cognitive concern had about the same effect in the general population. In people with HIV, dementia was rarely coded, so the effect size was not significant. Cognitive concerns expressed vocally in the year prior to a COVID-19 diagnosis were associated with an increased risk of death.
In summary, dementia and cognitive concerns are associated with the risk of mortality in COVID-19. If ICD billing codes are used across a population, we need to consider whether everyone is appropriately coded.
Q. What questions remain unanswered and what future studies are planned?
First, we need to validate these findings in a larger cohort that includes access to unstructured clinical notes as these will be important in people with HIV, and determine whether death and morbidity are more likely in these individuals. Another question is: how does pre-existing cognitive concern impact on post-COVID care and long-term function?
Q. What are the practical implications of this study?
I think it is important to recognize that dementia can be misclassified in a population. Large studies relying on ICD billing codes may underestimate disease burden related to dementia, with potential greater implications for people who may have cognitive impairment before the age of 65 years, such as people with HIV. It is important to identify which individuals are being missed, and this should affect the prioritization of resource allocation. We should consider incorporating unstructured clinical notes into clinical research, when annotating cohorts for the presence or absence of neurological diseases, such as cognitive impairment, among people with HIV.
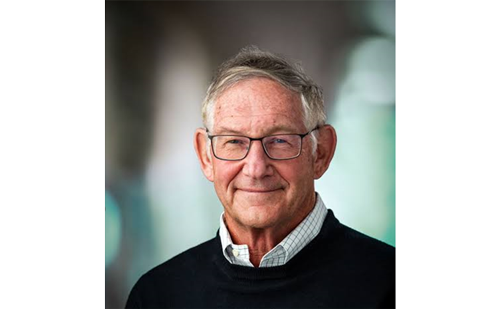
Shibani S Mukerji
Shibani S Mukerji is the Associate Director of the Neuro-Infectious Diseases Unit at Massachusetts General Hospital (MGH). Her clinical focuses are neuro-infectious diseases, with specific interests in neurological complications and aging in people living with HIV. She received her undergraduate degree from Yale University, and her MD and PhD (Neuroscience) from the Case Western Reserve University School of Medicine. She completed an internship in internal medicine at MGH and residency in neurology at the Mass General Brigham-Harvard Neurology Residency (MGH and Brigham and Women’s Hospital). Her lab focuses on systemic indicators of health, immune function and metabolite networks to advance our understanding and management of neurological disorders after infections.